|
Getting your Trinity Audio player ready...
|
When seemingly disparate symptoms—cognitive impairment, visual acuity loss, peripheral circulatory compromise, and inflammatory joint pain—coalesce in a patient, it signals a high probability of a single, underlying systemic disease process. These four domains, while managed by distinct medical specialties (neurology, ophthalmology, cardiology, and rheumatology), share a fundamental physiological dependency on vascular integrity and immune regulation. Therefore, their concurrent failure often points toward pathologies characterized by chronic, pervasive inflammation and endothelial dysfunction.
This expert analysis will delineate the clinical presentation of this tetrad, explore the primary differential diagnoses, explain the critical underlying pathophysiology, and propose comprehensive management strategies encompassing both conventional medical and evidence-based lifestyle interventions. Given the complexity of these interactions, we strongly recommend that patients experiencing any combination of these symptoms seek immediate consultation with a primary care physician who can initiate specialist referrals. Read this full analysis to grasp the interconnected nature of these symptoms and the urgency of multidisciplinary diagnostic assessment.
The Clinical Tetrad: Defining the Problem
The concurrent presentation of symptoms across multiple organ systems is inherently more serious than isolated dysfunction. Understanding the specific nature of each affected area is key to differential diagnosis. If these symptoms are recognized, timely referral to a rheumatologist, endocrinologist, or neurologist is often warranted.
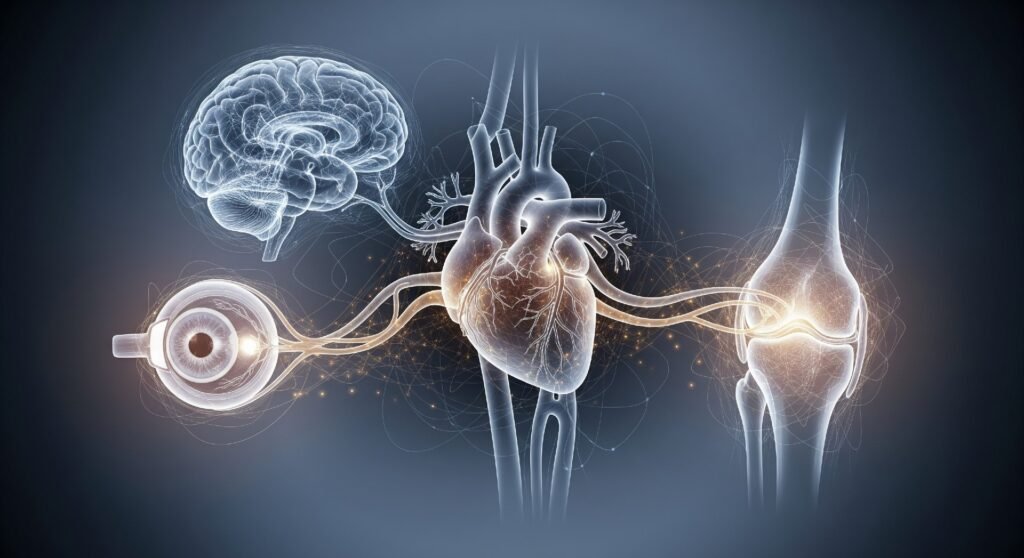
Cognitive Impairment and Memory Loss (CNS)
The manifestations often referred to as “brain fog,” mild cognitive impairment, or specific episodic memory deficits are highly prevalent in chronic systemic diseases. This is not simply age-related memory lapse, but a demonstrable reduction in executive function, processing speed, and attentional capacity. Impairment in this domain indicates compromised cerebral blood flow or chronic neuroinflammation.
Visual Acuity Decline and Ocular Changes (Vision)
Vision loss, typically progressive, often stems from microvascular damage within the retina (retinopathy) or inflammatory attack on the optic nerve (optic neuritis). Since the eye is rich in fine capillaries, it serves as a critical window into the state of the body’s microvasculature. Decreased visual acuity signals established, long-term vascular compromise. Any rapid or unexplained vision change necessitates an urgent ophthalmology consultation.
Poor Peripheral Circulation (Circulation)
Symptoms here include cold extremities, intermittent claudication (pain while walking), and non-healing ulcers. This sign indicates damage to both large vessels (macrovascular disease, such as peripheral artery disease) and small nerve fibers (microvascular neuropathy). A breakdown in circulation signifies a failure in the body’s delivery system for oxygen and nutrients.
Inflammatory Arthralgias and Joint Swelling (Joints)
Joint involvement ranges from non-erosive arthralgia (pain without destruction) to destructive chronic synovitis (true arthritis). The presence of symmetrical joint pain and morning stiffness is highly suggestive of an autoimmune or inflammatory etiology attacking the synovial tissues.
Unraveling the Etiology: Key Systemic Candidates

The presence of the clinical tetrad strongly narrows the diagnostic focus to a few well-documented systemic illnesses. A definitive diagnosis requires specialist input and comprehensive laboratory testing.
Uncontrolled Diabetes Mellitus (DM)
Diabetes—particularly when glycemic targets are not consistently maintained—is perhaps the most common single entity capable of generating this full spectrum of symptoms. It is a dual threat, causing both macro- and microvascular damage.
Type 1 DM is an an autoimmune condition resulting from genetic predisposition and environmental triggers, leading to the destruction of insulin-producing cells. Type 2 DM, the most common form, results from a complex interplay of genetic susceptibility, obesity, physical inactivity, and insulin resistance.
Hyperglycemia directly contributes to the accumulation of advanced glycation end products (AGEs), which stiffen vessel walls. This leads to:
- Vision: Diabetic retinopathy (microvascular damage to the retina).
- Circulation: Peripheral neuropathy (nerve damage) and peripheral artery disease (PAD).
- Memory: Uncontrolled DM is a robust predictor of cognitive impairment, as detailed in the study Type 2 Diabetes, Cognition, and Dementia in Older Adults: Toward a Precision Health Approach. Moreover, Type 2 DM is specifically associated with a significantly increased risk for dementia and impaired executive functions, a correlation strongly established in the review Diabetes and Cognitive Impairment.
- Joints: Diabetic arthropathy, including conditions like diffuse idiopathic skeletal hyperostosis (DISH) or limited joint mobility syndrome.
Systemic Lupus Erythematosus (SLE)
SLE is an archetypal autoimmune disease where autoantibodies target numerous organ systems, including the vasculature and connective tissues. Lupus is often dubbed “the great imitator” due to its variable presentation.

The exact cause of SLE remains unknown (idiopathic), but current evidence points to a combination of genetic susceptibility, hormonal factors (especially estrogen), and external environmental triggers such as ultraviolet (UV) light exposure, certain medications, and viral infections.
The systemic inflammation in SLE causes:
- Joints: Non-erosive arthritis, typically affecting the small joints of the hands and wrists.
- Memory: Neuropsychiatric SLE (NPSLE) can manifest as cognitive dysfunction (“lupus fog”), headaches, or even seizures. CNS involvement in SLE may occur in up to 75% of patients, according to the review Neuropsychiatric Manifestations in Systemic Lupus Erythematosus: Epidemiology, Pathophysiology and Management. The damage is directly due to cerebral vasculitis or autoimmune-mediated neural damage, with cognitive dysfunction reported in 30% to 50% of cases, as highlighted in a publication on Neuropsychiatric Symptoms in Lupus.
- Vision: Retinal vasculitis, where inflammation compromises the retinal blood vessels, potentially leading to acute vision loss.
- Circulation: Increased risk of thrombotic events (clots) due to associated antiphospholipid antibodies, severely impairing blood flow. Patients presenting with this presentation should be assessed by a rheumatology specialist.
Rheumatoid Arthritis (RA) and Connective Tissue Diseases
RA is fundamentally a disease of chronic synovitis but is a known systemic inflammatory disorder.
RA is an autoimmune disease where the immune system mistakenly attacks the lining of the joints (synovium). Its etiology involves a complex interaction between genetic risk factors (notably the HLA-DRB1 gene) and environmental factors, including chronic smoking and specific mucosal or periodontal infections, which trigger the autoimmune response.
- Joints: Chronic, destructive inflammation.
- Vision: Ocular involvement, such as scleritis (inflammation of the sclera), is common.
- Memory/Circulation: Chronic systemic inflammation in RA is a recognized independent risk factor for accelerated atherosclerosis (macrovascular disease) and is increasingly linked to cognitive decline through inflammatory pathways crossing the blood-brain barrier, as explored in the analysis Cognitive Decline in Rheumatoid Arthritis: Insight into the Molecular Pathogenetic Mechanisms. Studies show that high inflammatory activity in RA is associated with specific cognitive deficits, including impaired visuospatial and executive function, a finding detailed in the study Impact of inflammation on cognitive function in patients with highly inflammatory rheumatoid arthritis.
The Core Pathophysiology: Endothelial Dysfunction and Chronic Inflammation
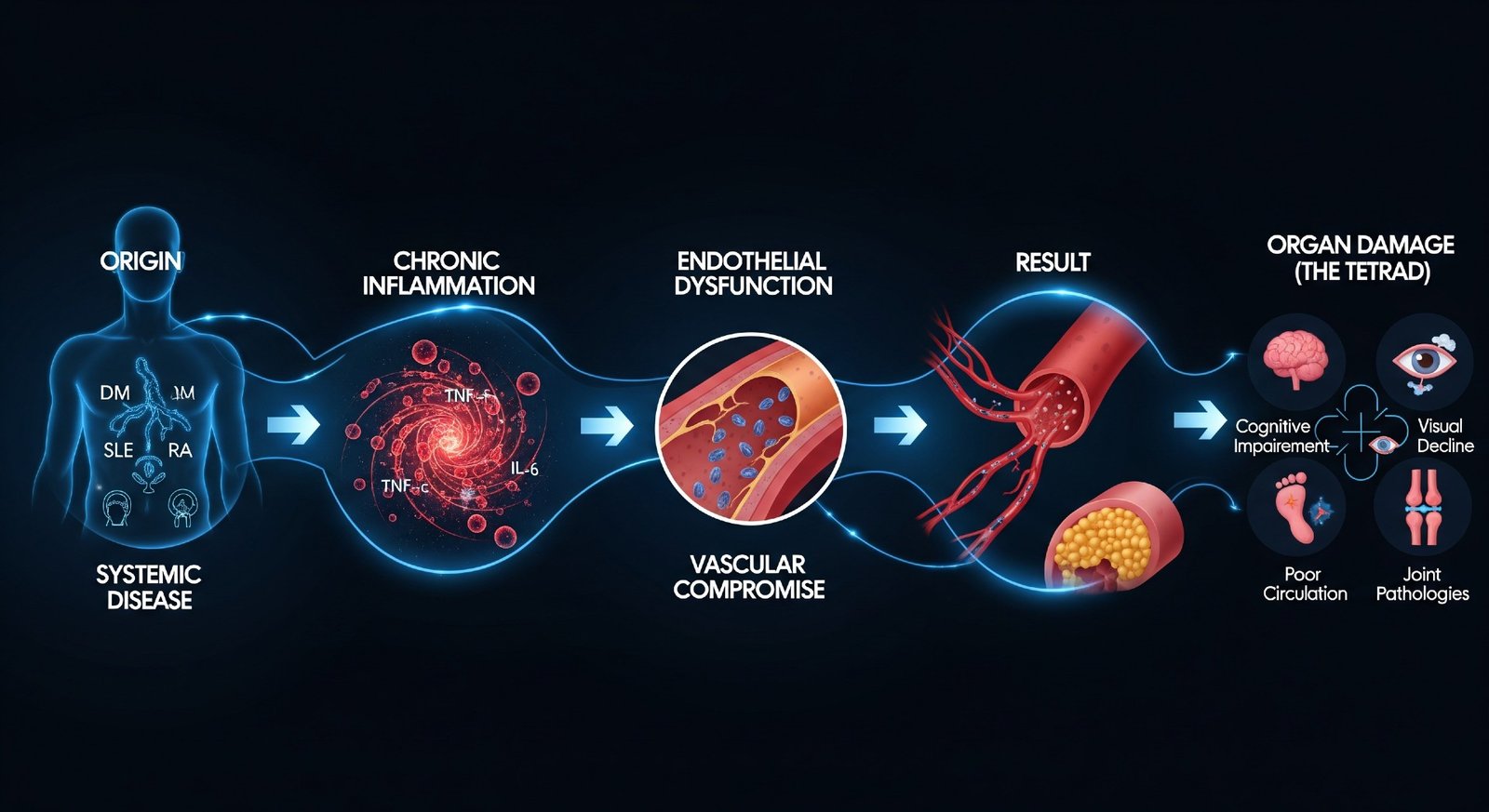
The common denominator connecting all four systems is the endothelial layer—the inner lining of all blood vessels—and chronic inflammation.
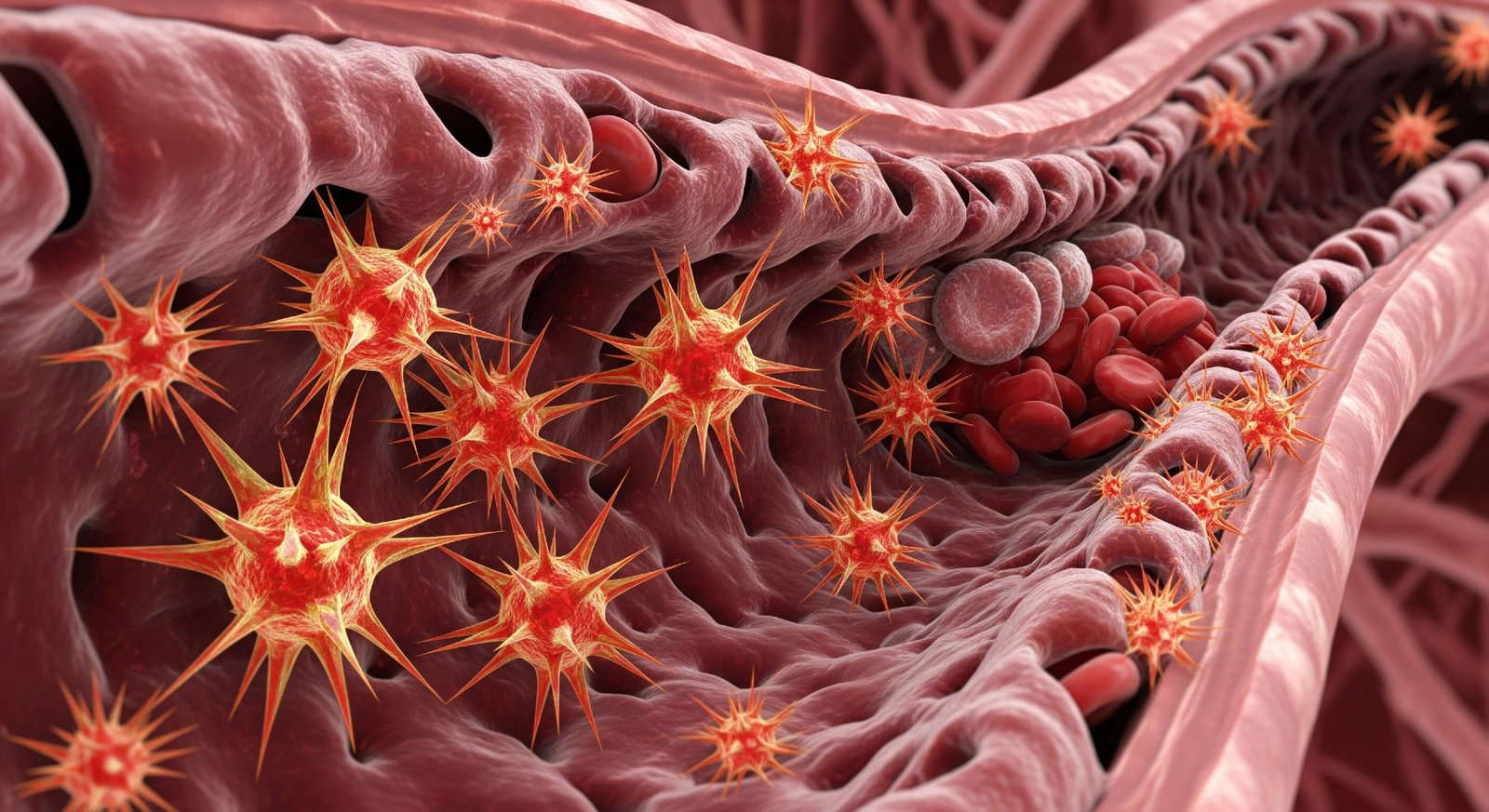
The Role of Endothelial Dysfunction
The endothelium regulates vascular tone, prevents coagulation, and controls the passage of substances into tissues. Systemic diseases like DM, SLE, and RA all initiate or perpetuate a state of endothelial dysfunction (ED). ED involves a reduced availability of nitric oxide (NO), leading to vasoconstriction and a pro-inflammatory state that allows plaque formation. Chronic inflammatory diseases, including autoimmune arthritis and lupus, are strongly associated with accelerated atherosclerosis and endothelial dysfunction, a relationship confirmed in the review Endothelial Dysfunction in Chronic Inflammatory Diseases and in the study Inflammation and endothelial dysfunction: intimate companions in the pathogenesis of vascular disease. When the endothelium is compromised, the body effectively ages faster, particularly in terms of its circulation.
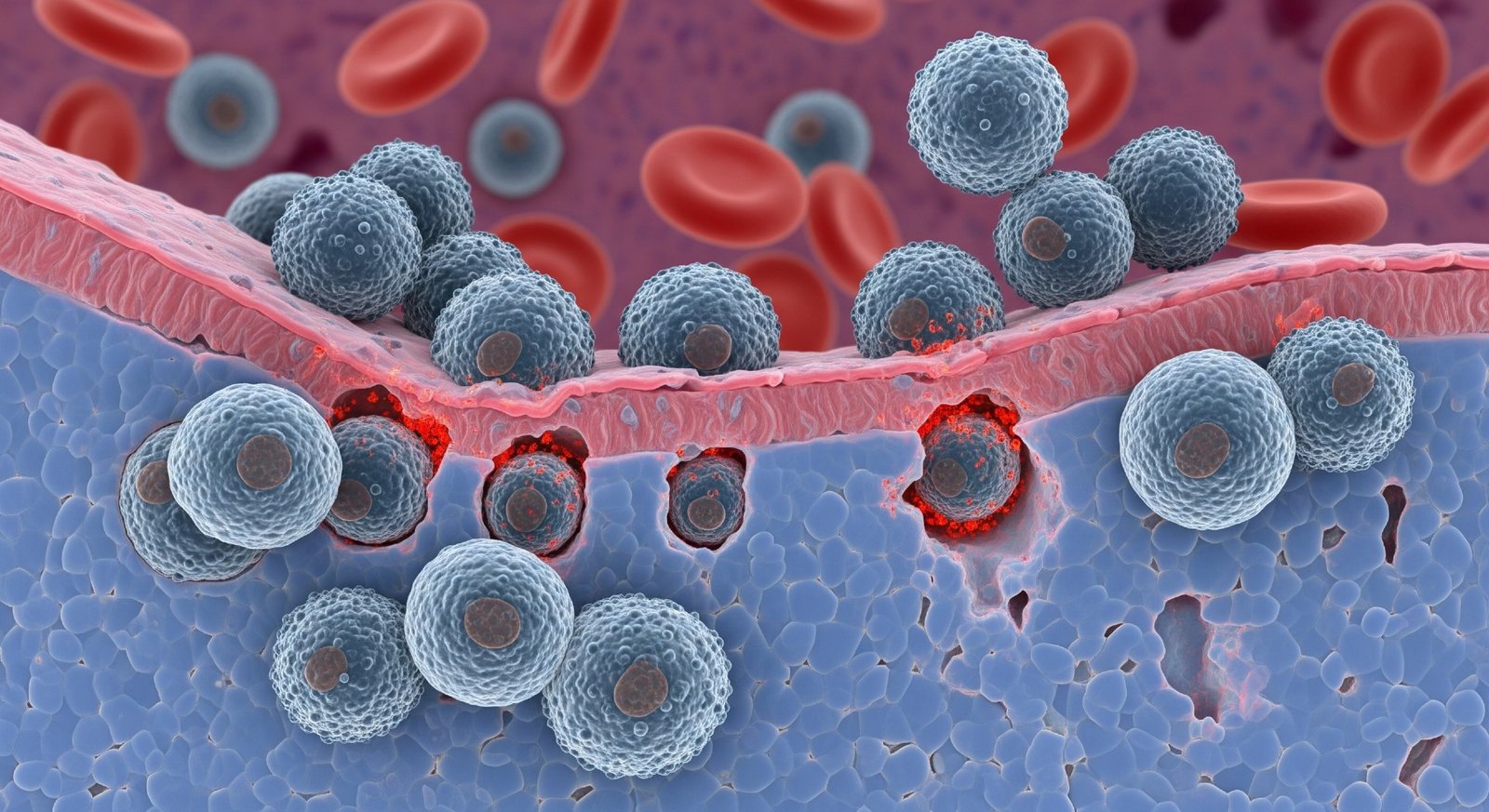
Microvascular Compromise
Microvascular compromise—damage to the smallest arterioles and capillaries—is the direct link to visual and cognitive decline. These vessels are essential for supplying the high metabolic demands of the retina and the cerebral cortex. Damage results in localized ischemia and tissue death, leading directly to retinopathy and vascular contributions to memory loss.
Inflammaging: The Systemic Cycle
Chronic, low-grade inflammation, sometimes termed “inflammaging,” drives this entire process. Inflammatory cytokines (e.g., TNF-α, IL-6) released in response to the primary disease (e.g., high glucose in DM, autoantibodies in SLE) circulate systemically. These molecules not only attack the joints, causing arthritis, but also cross the blood-brain barrier, triggering neuroinflammation and contributing to cognitive deficits.
Comprehensive Management Strategies
Management for patients presenting with this tetrad must be multidisciplinary and aggressive, focusing on controlling the primary disease, mitigating inflammation, and supporting vascular health. Effective treatment always begins with specialized medical guidance and accurate diagnosis.
Conventional Pharmacological Interventions
- Glycemic and Pressure Control (DM focus): For diabetes, rigorous control of HbA1c is paramount to slowing down microvascular progression in the eyes and nerves. Blood pressure control is equally critical to reduce vascular shear stress. An endocrinologist should manage all aspects of glycemic control.
- Immunosuppression (Autoimmune focus): For SLE and RA, treatment involves disease-modifying antirheumatic drugs (DMARDs) like Methotrexate, Hydroxychloroquine, and biologic agents (e.g., TNF inhibitors, B-cell inhibitors). These agents aim to halt the autoimmune attack and systemic inflammation. A rheumatology specialist must supervise this highly specialized treatment.
- Vascular Protection: Daily use of aspirin (as indicated for secondary prevention), statins for aggressive cholesterol management, and ACE inhibitors/ARBs for blood pressure are standard components of vascular risk reduction across all these conditions. Cardiology input is essential here.
Lifestyle and Natural Support
While not substitutes for conventional medication, lifestyle modifications are essential for long-term prognosis, particularly in reversing endothelial dysfunction and reducing inflammation. Always discuss these interventions with your treating physician or a registered dietitian.
- The Anti-Inflammatory Diet: Adopting a Mediterranean or similar diet rich in Omega-3 fatty acids (found in fatty fish), antioxidants (berries, leafy greens), and polyphenols (extra virgin olive oil) is crucial. These components directly counteract chronic inflammation and support NO production.
- Structured Aerobic Exercise: Regular, moderate-intensity aerobic activity (e.g., brisk walking, swimming) has been proven to improve endothelial function, increase peripheral circulation, and exert a neuroprotective effect on the brain, thus supporting memory.
- Targeted Supplementation:
- Omega-3 Fatty Acids (EPA/DHA): Potent anti-inflammatory properties benefit joints and vascular health. Dosing should be discussed with a physician.
- Alpha-Lipoic Acid: May offer neuroprotection and improve symptoms of peripheral neuropathy, particularly in diabetic patients.
- Vitamin D: Low levels are common in autoimmune diseases and are linked to generalized pain and inflammation. Optimization is recommended.
Bridging the Gaps: The Path to Multidisciplinary Management
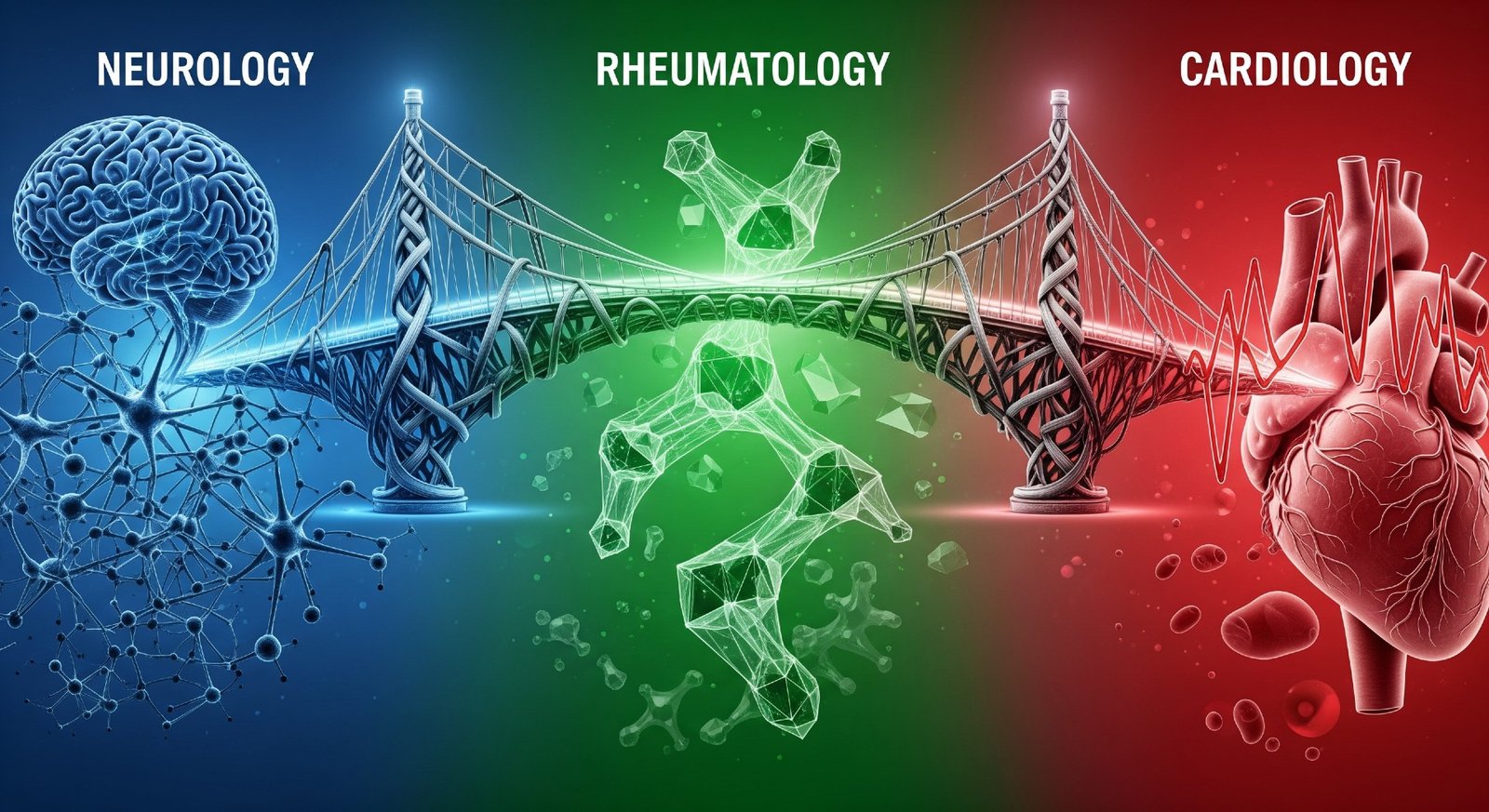
The simultaneous manifestation of problems in memory, vision, circulation, and joints is a powerful clinical indicator of systemic pathology, with uncontrolled diabetes mellitus and systemic autoimmune diseases like lupus and rheumatoid arthritis being the leading culprits. Clinicians must adopt a low threshold for diagnostic testing (including HbA1c, inflammatory markers, and specific autoantibody panels) when faced with this tetrad. Effective management depends on early diagnosis, aggressive control of the primary pathology, and a commitment to vascular protection through both advanced pharmacology and foundational lifestyle changes.
This is a dynamic area of medicine. What would your approach be if a patient presented with this constellation of symptoms? Remember, only a specialist can provide an accurate diagnosis and create a targeted treatment plan. We invite medical professionals and the public alike to share their insights and experiences in the comments below.